Moderna, Merck Vaccine Combo Cuts Melanoma Recurrence
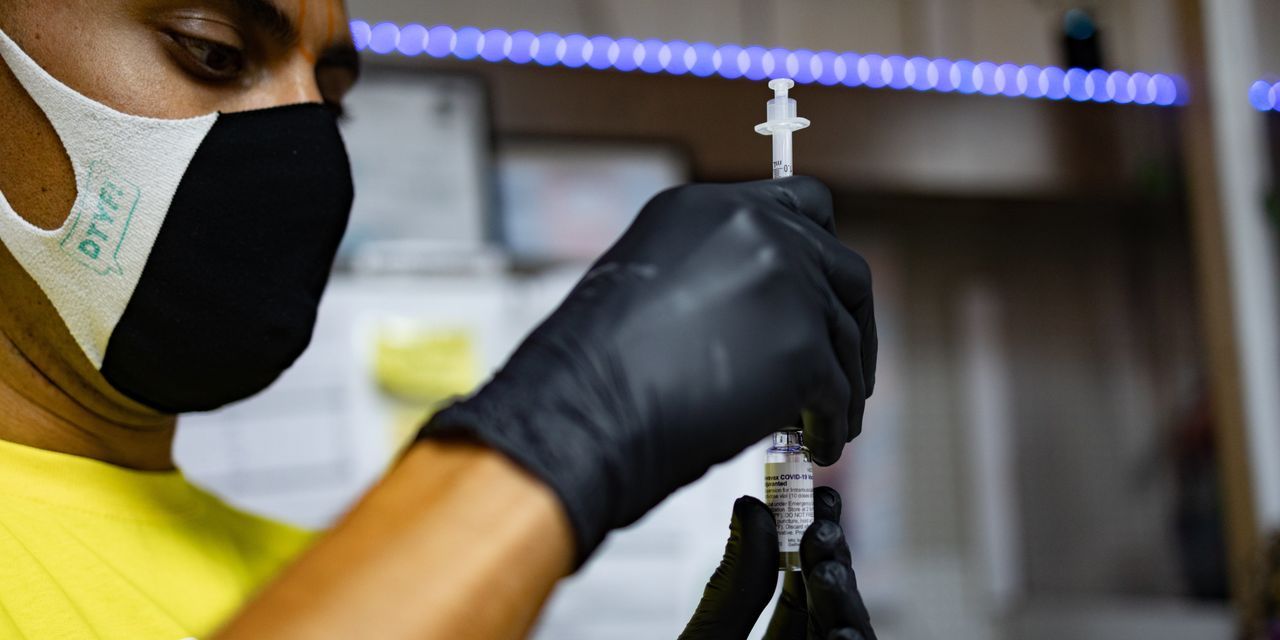
On Tuesday, Moderna and Merck announced their co-developed, personalized skin cancer vaccine — based on individual tumor DNA — significantly reduced skin cancer recurrence in patients with phase three or four melanoma who had tumors removed in surgery.
Facts
- On Tuesday, Moderna and Merck announced their co-developed, personalized skin cancer vaccine — based on individual tumor DNA — significantly reduced skin cancer recurrence in patients with phase three or four melanoma who had tumors removed in surgery.
- Patients who took a combination of Moderna's mRNA vaccine technology and Merck's already-approved Keytruda immunotherapy saw a 44% reduction in relapse and death compared to those who only took Keytruda.
- This comes after Merck agreed to jointly develop and sell the treatment in October, sharing costs and any profits equally. Keytruda, a so-called checkpoint inhibitor, is designed to disable a protein called programmed death 1, or PD-1, that helps tumors to evade the immune system.
- The roughly 150-patient phase-two trial began in 2019, with some patients receiving up to nine doses of the vaccine, given every three weeks in combo with Keytruda, for up to 18 cycles. The trial was delayed after the pandemic prompted Moderna to repurpose some of its cancer vaccine manufacturing to create COVID shots.
- The companies said that serious treatment-related adverse events occurred in 14.4% of patients who received the vaccine combination compared to 10% in those who only received the immunotherapy, adding that Keytruda already has some known side effects.
- Shares of Moderna jumped 23% in midday trading on Tuesday, with Merck shares seeing a nearly 1% jump. A final phase three trial is expected to start next year, the final round before the companies submit the drug to regulators.
Sources: CNBC, Wall Street Journal, Reuters, CNN, and CBS.
Narratives
- Narrative A, as provided by The Washington Post. Cancer vaccine research hasn't been very successful due to cycle times taking too long, which is why this study is such a breakthrough. The use of mRNA technology not only allows a quicker process but a personalized one in which individual patients' tumor DNA can be used to attack specific cancer cell mutations harming their immune systems.
- Narrative B, as provided by Frontiers. This is all positive news, but we shouldn't get ahead of ourselves over just one headline. While promising, potentially successful cancer vaccines like this face many challenges and are still years away from being rolled out. Further research is needed.